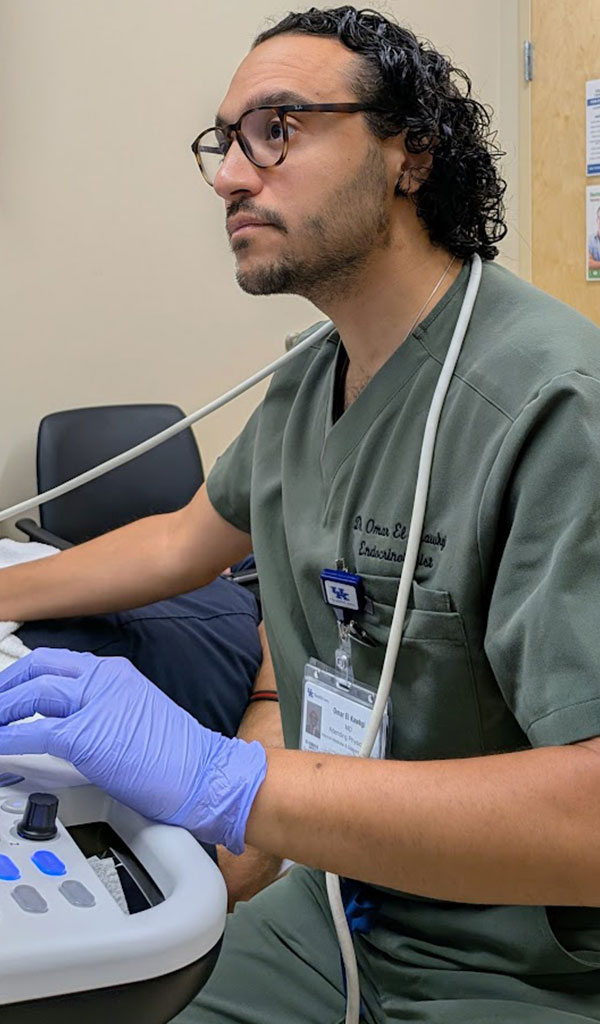
Omar M. El Kawkgi, MD, leads the building of UK Healthcare’s Markey Cancer Center’s thyroid cancer program
LEXINGTON Endocrinologist Omar M. El Kawkgi, MD, joined the University of Kentucky Markey Cancer Center in July of this year, 2025. His reason for coming is reminiscent of the famous line from the movie, Field of Dreams: “If you build it, they will come.” The difference is, El Kawkgi came not because it was built, but to do the building himself.
“I was at a point in my career where I wanted to start thinking about how I could leverage my perspective on thyroid cancer on a greater level,” El Kawkgi says. “I was looking for a place where I could create and develop a thyroid cancer program, and UK was looking for that person.”
El Kawkgi came to Kentucky from the Mayo Clinic in Rochester, Minnesota, where he completed a fellowship in endocrinology. After his fellowship, he remained at the Mayo Clinic for a few years as an assistant professor of medicine.
While he never expected to come to Kentucky, El Kawkgi is no stranger to a change of scenery.
“I was fortunate to grow up in a diverse and multicultural environment,” he says. “I was born in Egypt, raised in Toronto, Canada, and spent my summers in Egypt where I learned Arabic and developed a deep appreciation for Middle Eastern culture. My family moved frequently in my adolescent years, and I had the opportunity to spend parts of my childhood in Atlanta and Abu Dhabi as well.”
El Kawkgi completed his undergraduate degree in biomedical science at the University of Ottawa, then attended medical school at the Royal College of Surgeons in Dublin, Ireland. He completed his residency in internal medicine at the University of MassachusettsBaystate Medical Center before joining the Mayo Clinic.

University of Kentucky Markey Cancer Center in
July of 2025.
He comes from a medical family. His uncle is an internist and his great aunts and uncles all practiced in medicine. Additionally, El Kawkgi’s aunt is a pediatric medical oncologist in Egypt.
“My aunt has been my inspiration since childhood,” he says. “I recall her unwavering dedication to her patients, no matter the time of day. I will never forget when a young man approached her in public to thank her for her care years after she was involved in the diagnosis and treatment of his childhood cancer. That moment left a lasting impression on me because it showed the profound and lifelong impact a physician can have on a patient’s life, far beyond the walls of the hospital. This continues to inspire me to strive for that same level of compassion and commitment in my own career, reminding me that every interaction has the potential to make a meaningful difference.”
The Lure of Endocrinology
Drawn to endocrinology early in his training, El Kawkgi receives satisfaction in diagnosing and treating thyroid cancers. It is a challenging specialty with a wide range of presentations and outcomes.
“I am a big picture thinker, and endocrinology often involves multiple organ systems and requires connecting seemingly unrelated symptoms into a cohesive diagnosis,” he says. “I was intrigued by thyroid cancer because it is a disease with such a wide spectrum of presentations. It can vary in the age of the people who come to see me, in their background, and in terms of their disease. It varies from indolent micro-papillary cancers that may sometimes need only surveillance to aggressive anaplastic cancers requiring intensive, multidisciplinary care. Each case is unique, and it challenges me to partner with my patients to tailor a treatment plan that fits their disease and their lives.”
Detection and Treatment
El Kawkgi says most thyroid cancers are detected incidentally by primary care providers, ENTs, general surgeons, and even dentists. He adds that the cancer is more likely to present in women than men and is most commonly found in asymptomatic patients ages 20 to 40. He estimates that he sees between five and ten new cases of thyroid cancer per week. This aligns with national numbers that demonstrate an increase in the incidence of thyroid cancer over the last few decades.
“We did some studies when I was with Mayo Clinic, and we found that, although the incidence has increased, the mortality from thyroid cancer has not,” El Kawkgi says. “In fact, it’s been quite steady, suggesting to us that there may be an increase in detection as opposed to an increase of the actual pathology.”
Fortunately, mortality rates for thyroid cancer are low compared to many other cancers. El Kawkgi points out that the vast majority of thyroid cancer patients have very positive outcomes, with an approximate survival rate of 98 percent at five years after diagnosis. Additionally, the recurrence risk is generally low and varies between 1% and 10% in most cases but can be as high as 30%.
El Kawkgi sees patients who have already been diagnosed and those who are referred to him for diagnosis. In both cases, his first meeting with the patient is important and focuses on educating the patient and understanding their needs and concerns with an emphasis on shared decision-making.
“Very frequently in this field, there is no one right answer. We operate in the gray,” he says. “Not every treatment for one patient is going to look the same as for another patient. We are at a stage where we are starting to understand how to stratify patients based on their particular disease, their particular situation, and design a treatment that works for them. When we do it that way, we see improvement in outcomes because we avoid burdening patients with treatments they may not need.”
El Kawkgi is in the early stages of building his medical practice at UK HealthCare and sees 15 to 25 patients per week, with additional time divided between clinic, teaching fellows, and other administrative duties. He also serves as an associate editor for the Journal of Clinical Thyroidology.
“I am fortunate to work with a highly collaborative team at UK,” he says. “I collaborate
closely with surgeons, oncologists, radiologists, pathologists, and nuclear medicine teams among others. It takes a village to take care of thyroid cancer patients.”
Treatment Options
Despite the relatively low mortality and recurrence rates, the detection and treatment of thyroid cancers can be quite complicated and vary from patient to patient. For patients who have undergone successful treatment, the focus is on monitoring it for recurrence. Sometimes that means surveillance only, while other patients might be at higher risk and in need of preventative measures or treatment such as radioactive iodine.
“The important part of my job is to help identify patients who do not have that favorable prognosis so that we can utilize various treatment strategies in that subgroup,” El Kawkgi says.
He points to advancements that help prevent over-diagnosis. For instance, high-resolution ultrasound can aid in the creation of risk stratification scores based on the sonographic characteristics of thyroid nodules. This helps identify which nodules do, and do not, need to be biopsied.
“Molecular profiling and genetic testing are now routinely used in this space,” he adds. “It’s particularly useful when the biopsy results are indeterminate to help us decide where to go from here.”
Patient input can be a deciding factor as well. El Kawkgi shares the story of a patient who was an opera singer. After the initial procedure, she expressed concern about additional surgeries and potential damage to her vocal cords.
“With multi-disciplinary input we were able to design a treatment plan that accounted for her circumstances, while still monitoring her risk of cancer recurrence appropriately. By doing that we were able to save her from having surgery, and I think that had a very large impact on her life,” he says. “What drives me is to remember that the patient in front of me is more than a diagnosis. When I approach care that way it gives me immense satisfaction to be able to see how I can have a positive impact on people’s lives.”




