Kentucky Bone & Joint Surgeons excels as an independent orthopedics and sports medicine practice by attending to details and providing customized care
LEXINGTON Is a four-doctor medical practice that is physician owned and managed, with fellowship-trained orthopedic surgeons, sustainable? “Yes, absolutely, if they have a solid foundation of highly motivated physicians, PAs, and administrative staff and continue to provide optimal patient satisfaction and outcomes,” says Kaveh Sajadi, MD, managing partner for Kentucky Bone & Joint Surgeons.
We provide exceptional, patient-focused, individualized, cutting edge orthopedic and sports medicine care. That’s why we’re successful, even in a challenging fiscal environment where insurance companies pay hospital-based healthcare systems more than they reimburse private practices for the same procedures.”
Founding Father and Son
Kentucky Bone & Joint Surgeons was founded by Kooros Sajadi, MD, as a sole practitioner practice. His son Kaveh joined the practice after his fellowship training in 2006. Kaveh took over as managing partner in 2012 when Kooros retired.
“Being the managing partner gives me the view behind the curtain in the business of healthcare, making me a better steward of cost-effective healthcare,” says Sajadi.
Kaveh Sajadi, MD, grew up in Lexington and received his undergraduate degree from Vanderbilt University and medical degree from the UK College of Medicine. He completed his orthopedic surgery residency at the prestigious Campbell Clinic-University of Tennessee, and then did a fellowship in shoulder and elbow surgery at the Hospital for Joint Diseases-NYU

Medical Center, where he met and trained under Dr. Joseph Zuckerman, MD, an internationally recognized expert in shoulder surgery.
I’ve stayed in contact with Dr. Zuckerman throughout my career. We talk five or six times a year. He was a great teacher and continues to be an inspiration to me,” says Sajadi.
What’s New in Shoulder Replacement?
The shoulder is the body’s most complex joint, with the widest array of motion and use, says Sajadi. “I chose to specialize in shoulder because I like to work with my hands and my mind. I get the satisfaction of working with multiple generations of patients, from adolescents to mature seniors. It may be a cliché, but I like seeing my patients get better and fixing their problems.”
Shoulder replacement and repair continues to innovate. Sajadi employs both the reverse shoulder and the subscapularis sparing techniques when appropriate. Computer assisted mapping gives Sajadi real-time input on where to make the cuts on the more challenging presentations of bone deformities.
“Computer-assisted surgery helps a surgeon stay in a very narrow range when making cuts on the humerus, lowering the chance for replacement failure and additional surgeries,” says Sajadi.
Biologics continue to offer new treatments, both platelet-rich plasma (PRP) and xenograft transfer of bovine tendon tissues, says Sajadi, who has designed a shoulder joint replacement product now in trials and seeking FDA approval, possibly ready for market in the fourth quarter of 2025. “We’ve been working on it for a long time,” he says.
In addition to meeting patients in clinic, with surgery two days a week, administrative duties as managing partner, consulting, and designing new shoulder parts, Sajadi also has a faculty appointment at UK where he teaches some of the finer points of shoulder surgery to fifth-year UK orthopedic residents and sports medicine fellows. “Even if they don’t become

shoulder surgeons, I hope my teaching will make my students and fellows better orthopedic doctors,” he says.
On the horizon for Kentucky Bone & Joint is adding a hand specialist and hip-replacement surgeon. “We are actively recruiting for those positions and are talking with several fellows and residents now,” says Sajadi.
Meet Samuel Coy, MD
Samuel Coy, MD’s, roots are deep in Central Kentucky medicine and agriculture. He says his father, James Coy, MD, practiced orthopedics so he could support his other passion, the family farm, which had been in the family for generations, first as a tobacco farm and more recently raising beef cattle.
Coy shadowed his father during his youth and embraced the dual roles of physician and farmer. Coy wore a leg brace as a child for a club foot, before becoming a high school and college athlete as a swimmer. Orthopedics has always been a part of his life.
Coy himself still works the farm whenever possible, so it’s no surprise that a memorable patient was a farrier, a blacksmith, who came to see him recently for a knee fracture he sustained when he fell while working out.
“I am amazed by what some patients can do when they’re highly motivated,” says Coy. “My patient needed to get back to work as soon as possible even though his work involved being on his knees. We repaired the kneecap fracture and set up his post-op rehab plan with physical therapy, and within months he was jogging and working again with his horses.”
Coy grew up in Richmond, Kentucky, received his BA in religious studies from Centre College, and studied abroad in London, Israel, and Ecuador. He received his medical degree from Vanderbilt University’s School of Medicine, completed his orthopedic surgery residency at the University of Chicago, and took fellowship training at the Steadman Hawkins Clinic of the Carolinas before returning to Kentucky in 2009 to join Kentucky Bone & Joint Surgeons where he is a partner.
“My training and studies gave me opportunities to live in larger cities for a while, but I always knew that I would settle in Central Kentucky to raise a family while being close to my family and the farm. All that plus working

in a private, physician- owned orthopedic and sports medicine practice is the best of both worlds,” he says.
The Knee Doctor
Being the knee specialist at Kentucky Bone & Joint Surgeons gives Coy a wide patient population, from young athletes with sports inju-
“Being an orthopedic surgeon and sports medicine doctor is a perfect fit for me.” — Daniel Hackett, Jr., MD

ries and adult worker’s comp cases, to mature individuals who need nonoperative therapy or joint replacement.
“The initial patient interview is so important and vital in deciding how to proceed,” says Coy. “We pride ourselves on providing personalized, patient-focused, customized orthopedic care. Dr. Sajadi makes that the goal of Kentucky Bone & Joint. We’re not the biggest practice with the highest patient volume, so we can take our time with each patient,” he states. Multiple trends are emerging in orthopedics and sports medicine, says Coy. Three that he sees most frequently are the growth of outpatient joint replacement surgery; computer-assisted navigation in knee surgery; and nonoperative remedies for joint repair such as PRP.
“The need for joint repair and replacement among baby boomers is growing exponentially. I don’t see it stopping,” says Coy. “People want to stay active. With new weight loss medications and innovations in arthroscopic surgery, there will never be a shortage of patients.”
Meet Daniel Hackett, Jr., MD
Complex shoulder replacement and repair are Daniel Hackett, MD’s, forte, an interest that he believes stems from working with his grandfather in his wood shop while growing up in Alabama. “I liked working with my hands and learned wood crafting from my grandfather. I played sports in high school and college. Biology and the human body and the skeletal system made sense to me. I knew in high school that I wanted to be a doctor and was drawn to orthopedics in medical school. Being an orthopedic surgeon and sports medicine doctor is a perfect fit for me,” says Hackett.
Shoulder replacement, including both anatomic and the reverse shoulder procedure and rotator cuff repair “are the bread and butter” of his practice, says Hackett. He also performs scapular reattachment and winging surgery, plus tendon transfers and sternoclavicular abnormalities.
He recalls a patient who, after a motorcycle injury and nonoperative repair for his shoulder, developed a scapular malformation and almost complete loss of use. Hackett used 3D printing to create a new shoulder joint, which restored the patient’s shoulder’s structure and function. “We recreated the shoulder joint he was missing and returned him to a normal life,” says Hackett.
Hackett’s patient population falls into two categories, common for orthopedic surgeons: the sports injury in adolescents to those in their mid-thirties, and the chronic arthritic pain patients who are sixty plus years old. “Bad luck or a lot of birthdays bring me my patients,” he says.
Losing Sleep and Function over Shoulder Pathology
If there is a gender bias in shoulder repair and replacement, it seems to point toward young males and older women, says Hackett. “I see sports and work or trauma injuries among young men, then chronic pain and joint degradation among senior women,” he says. Among the geriatric population, loss of function and sleep are usually the final motivation.
My older female patients tell me that not being able to do simple things like reaching for a coffee mug on the cupboard’s second shelf because they can’t lift their arm really affects their quality of life,” says Hackett.
Not being able to sleep at night because of shoulder pain also brings patients to Hackett who says the debilitating effects of impaired shoulder pathology has effects beyond what one might think. “Not being able to sleep because my patients have shoulder pain causes them both mental health distress and potentially cardiovascular problems,” he says.
Innovation in Shoulder Replacement and Repair
Preoperative computer mapping is one of the innovations in shoulder replacement and repair and “gives me a leg up in surgery,” says
Hackett. Knee replacement surgeons have been using computer mapping for some time, but it is now coming into use in shoulder surgery
Hackett points to some additional innovations in shoulder replacement as game-changers and potential game-changers. The reverse shoulder technique, “putting the ball of the joint in the socket rather than at the head of the humerus, was huge for shoulder replacement,” says Hackett. He uses the reverse shoulder technique when the head of the humerus has abnormal wear due to stress on the joint when the rotator cuff has failed. He is likewise enthused by the subscapularis sparing approach in shoulder replacement, which he uses to avoid taking down the rotator cuff tendons during shoulder joint replacement surgery. This dramatically enhances recovery and limits restrictions after shoulder surgery, allowing patients to remove their sling the day after surgery and get back to their normal life in a much more rapid manner.
Hackett continues, “We’re scratching the surface of what biologics and platelet-rich plasma will add to nonsurgical orthopedics. Our practice is driven by research and evidence-based results, so we use it in applications that have data supporting its use.”
Hackett joined Kentucky Bone & Joint Surgeons in 2017 and is a partner in the practice.
“I wanted to learn a new skill set that was not being widely covered in our area.” — David A Hamilton, Jr., MD
Meet David Hamilton, MD
Foot and ankle are not the most-widely chosen specialty areas by orthopedic surgeons, but David A. Hamilton, Jr., MD, says, “I wanted to learn a new skill set that was not being widely covered in our area. My wife and I wanted to live in Lexington. It was a win-win situation for us.”
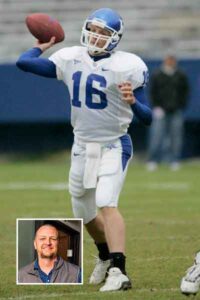
Hamilton grew up in Lexington, attended Tates Creek High School, and received his undergraduate degree at UK where he was a walk-on quarterback for the UK football team. He completed an MBA at the UK Gatton College of Business Administration before medical school at the UK College of Medicine. He completed a residency in orthopedics at UK followed by a fellowship in foot and ankle at the University of Pittsburg Medical Center. Hamilton credits several mentors at UK orthopedics for guiding and inspiring him, including Ray Wright, MD, Eric Moghadamian, MD, Darren Johnson, MD, Carter Cassidy, MD, and Jeff Selby, MD, outgoing chair of the orthopedic department. “Nobody’s clinical practice is perfect, but Dr. Selby’s approach is the probably the closest I’ve seen,” says Hamilton. “He’s a great doctor and teacher. He taught us that when there is an easy or difficult way to do things, the more
difficult path for the doctor is usually best for the patient. I’ve found that to be more and more true the longer I’ve practiced.”
Hamilton joined Kentucky Bone & Joint in 2021. His patient volume is expanding as is his coverage area, which encompasses Lexington and the surrounding cities of Paris and Winchester. His patient cohort is adolescent to adult with the common variety of sport related injuries, fractures, flatfoot deformity, plantar fasciitis, and Charcot foot deformity. He has a particular interest in bunion deformity, most commonly in women, for which he performs three dimensional and minimally invasive bunion correction.
Limb salvage and diabetic foot disease are a growing component of Hamilton’s practice. Employing new technologies, Hamilton says he uses amniotic allografts from umbilical cord tissue to facilitate wound care. “Diabetes is a major health concern in Central Kentucky, leading to many complications including amputation. Patient mortality increases dramatically when diabetic wounds and infections lead to amputation. Out of necessity, I’ve tried to develop a more comprehensive skill set to help prevent those negative outcomes,” says Hamilton.
Hamilton is bringing a charitable program that he participated in while in Pittsburgh to Kentucky. His fellowship mentor in Pittsburgh, orthopedic surgeon Stephen Conti, MD, along with his son Matt, formed “Our Hearts to Your Soles” in 2004. The purpose of the organization, which has been spreading across the country, is to provide those less fortunate with shoes and free foot examinations.
“Dr. Conti has collaborated with different shoe retailers to offer homeless people in Pittsburgh boots and shoes prior to the winter months,” says Hamilton. “Traditionally his fellows have taken that program to their home communities, and that’s something I’m going to do in Kentucky.”
Hamilton recently reached an agreement with Red Wing Shoes, which will donate shoes and boots to the Kentucky chapter of Our Hearts to Your Soles. Donations will start this holiday season. More information will be available on the Our Hearts to Your Soles website: www.heartstosoles.com In his spare time, Hamilton coaches his daughter’s flag football team and the chess club at Christ the King School in Lexington.
Fellowship Training
Kentucky Bone & Joint Surgeons will soon be the host site of a foot and ankle fellowship program, says Hamilton. He applied for the program through the American Orthopedic Foot and Ankle Association (AOFAF), and his application was accepted. He projects that fellowship training will begin in 2026.
“After five years of working in this specialty, I feel that I have something to offer to orthopedic residents who want to pursue the subspecialty of foot and ankle. We’ll be interviewing fellowship candidates this fall,” says Hamilton.
Managing partner Sajadi says that having a fellowship program at Kentucky Bone & Joint Surgeons will enhance the practice’s regional and national stature and coalesces well with the practice’s goal of teaching and training the next generation of orthopedic surgeons.
In Conclusion
The four fellowship-trained orthopedic surgeons at Kentucky Bone & Joint Surgeons are a unique mix of doctors. All of them played sports in high school or college and were drawn to the specialty because of a common passion to help their patients return to normal everyday activity, either through surgery or nonsurgical therapies.
All four expressed their shared joy in working with their hands and fixing patients’ problems, restoring function, and relieving pain and discomfort. Being part of a physician-owned private practice gives them input into how the practice is run, flexibility, and work/life balance, even with the additional responsibilities that come with the territory.
Is it sustainable? Absolutely, says Sajadi.
