FRANKFORT The recent change in the U.S. Preventive Services Task Force (USPSTF) guidelines to start colorectal cancer (CRC) screening at age 45 gives us an enormous boost in our ability to reduce the incidence and severity of CRC with simple changes to our best practices. In May 2021, the USPSTF released their final recommendation statement1 on the new screening age of 45, and it has gained momentum throughout the medical and social communities. New messaging that targets adults at age 45 has already begun, but perhaps the most impactful step in the process could be the direct messaging from healthcare providers to patients,2 stating that there are simple and affordable screening options for those at average risk for CRC, steps that take only minutes in the form of stool-based tests completed at home. By starting the conversation and encouraging the screening at an early age, ideally at age 35, the incidence of CRC can be reduced. They additionally recommend that the screening message should be repeated at least three to four times before the recommended age of initiation.3 The new motto with regard to screening is “45 is the new 50”. Providers should initiate screening messages with:
- a review of pertinent family history regarding CRC,
- a review of the importance of on-time screening and primary prevention for those with a family history, and
- a discussion of the screening options available to identify a risk-appropriate and value-concordant preference.
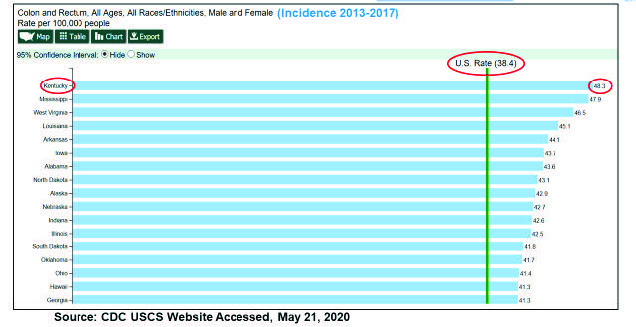
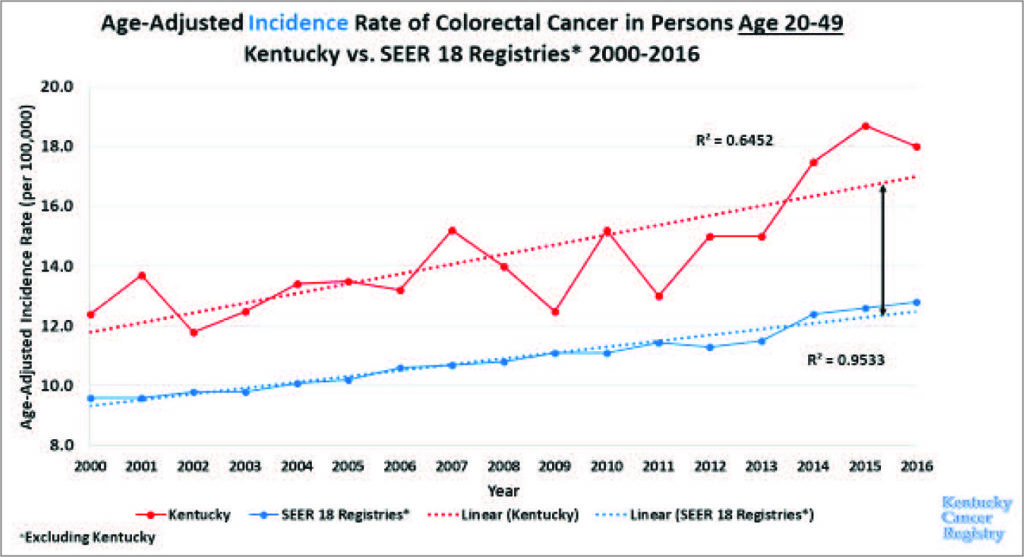
In an article published early in 2020, the investigators cited data from a review of Surveillance, Epidemiology, and End Results (SEER) registries and found that there was a significant increase in CRC in individuals between the ages of 49 and 50, indicating that these results “would be consistent with high rates of preexisting, undetected cancers in younger patients.” CRC incidence rates in individuals younger than 50 years of age may be underestimated, ultimately resulting in the patient “receiving a [potentially delayed] diagnosis of colorectal cancer after undergoing screening at 50 years.”4 Additionally, recent CDC US Cancer Statistics data show that Kentucky has the highest incidence rate of CRC in the nation (Figure 1).5 This supports the great need for Kentucky health care providers to be leaders in promoting the importance of CRC screening and of screening uptake in younger individuals. Companion data from 2000–2016 supports the importance of CRC screening in younger populations, as the data show there is an increase in CRC incidence in the Commonwealth in younger populations (Figure 2).6
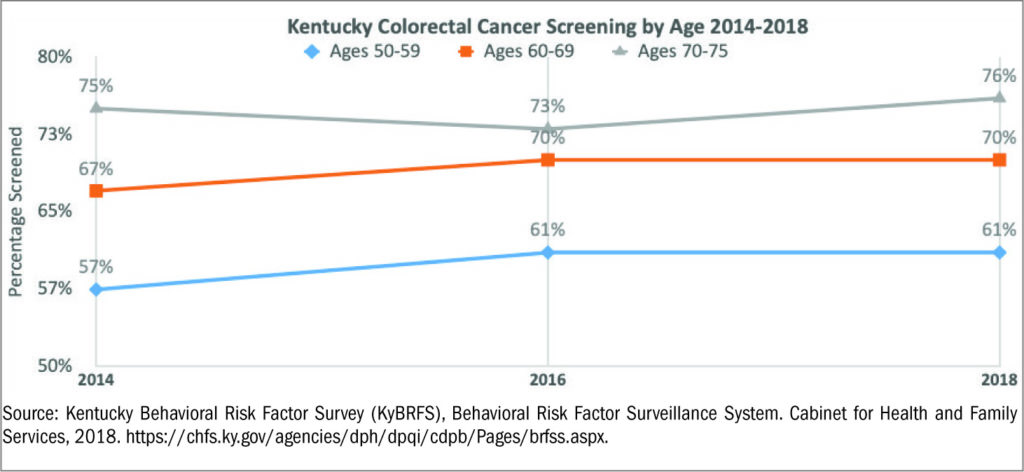
Between 2014 and 2018, Kentucky has had screening progress across populations aged 50–75, but the screening gap in younger populations, who are between the ages of 50–59, is significantly lower than older populations. The marginal upward trend in screening rates for those aged 50–59 from 2014 to 2018 was an increase of about 4%. However, in 2018 the average screening rate for an individual aged 60–69 was approximately 70%, and for those who were 70–75 years of age it was 76%. As of 2018 data displayed in Figure 3, individuals in Kentucky who were 50–59 years of
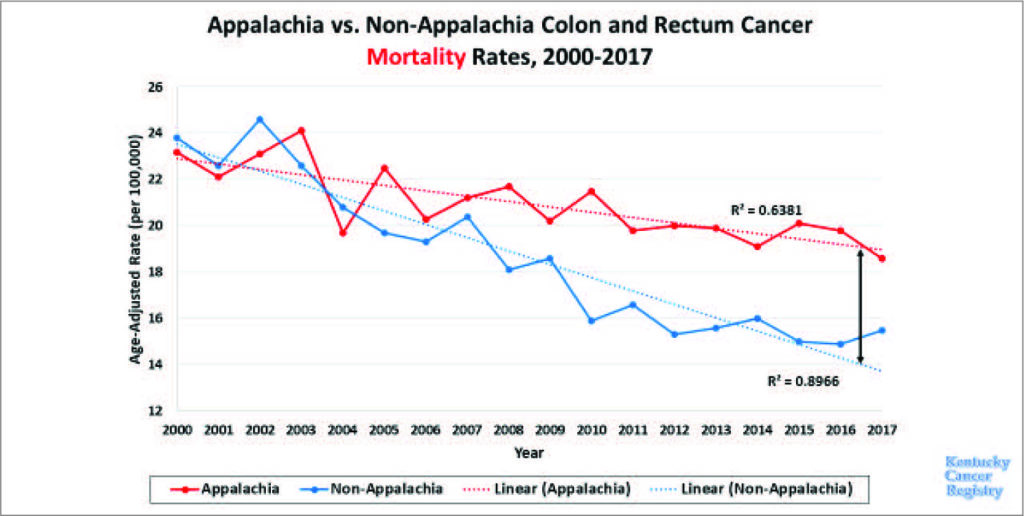
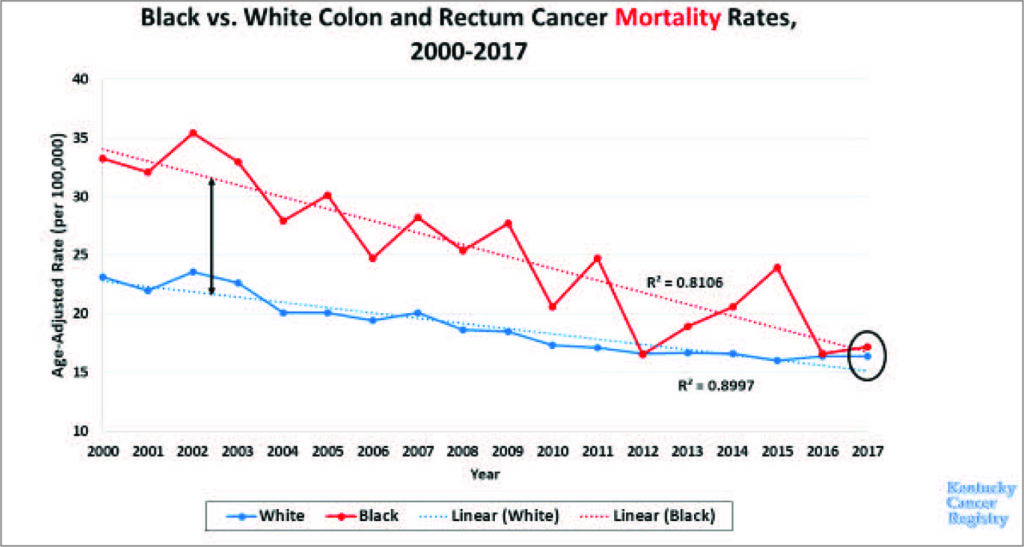
age had a CRC screening rate of only 61%.7 It would be appropriate to estimate that screening rates for those who are younger than 50 would be even lower. Due to the high rate of CRC mortality in the state, and the even higher CRC mortality in the state’s sub-populations, such as those who live in the Appalachian region (Figure 4) and those who are African-American (Figure 5),8 it is clear that screening younger populations is key to help decrease CRC incidence and mortality rates in the Commonwealth.
In an effort to encourage screening take-up in all populations in the Commonwealth, three simple practice modifications could be impactful:
- Talk about CRC screening early—don’t wait until age 45. Encourage individuals to gather and discuss family history.
- For patients at average risk, discuss various simple, affordable, and faster screening options, and encourage completion, including FIT and stool DNA (Cologuard).
- Prioritize colonoscopy referrals for those with increased risk due to personal or family health history.
1USPSTF Final Recommendation Statement, 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening
2Dyer et. al. Patient-Reported Needs Following a Referral for Colorectal Cancer Screening, 2019. https://doi.org/10.1016/j.amepre.2018.08.017
3Jones et al. Improving On-Time Colorectal Screening Through Lead Time Messaging. Cancer, 2020. https://acsjournals.onlinelibrary.wiley.com/doi/epdf/10.1002/cncr.32535
4Abualkhair et al. Trends in Incidence of Early-Onset Colorectal Cancer in the United States Among Those Approaching Screening Age. JAMA Network Open. 2020;3(1):e1920407. doi:10.1001/jamanetworkopen.2019.20407.
5Centers for Disease Control and Prevention US Cancer Statistics. 2020. https://www.cdc.gov/cancer/uscs/index.htm
6Kentucky Cancer Registry Incidence and Mortality Data 2017 https://www.kcr.uky.edu/ and Surveillance, Epidemiology, and End Results Data, National Cancer Institute 2017. https://seer.cancer.gov/data/
7Kentucky Behavioral Risk Factor Survey (KyBRFS), Behavioral Risk Factor Surveillance System. Cabinet for Health and Family Services, 2018. https://chfs.ky.gov/agencies/dph/dpqi/cdpb/Pages/brfss.aspx
8Kentucky Cancer Registry Incidence and Mortality Data 2017 https://www.kcr.uky.edu/ and Surveillance, Epidemiology, and End Results Data, National Cancer Institute 2017. https://seer.cancer.gov/data/