
By federal law, colorectal cancer (CRC) screening is a zero-cost sharing service for patients as defined in The Affordable Care Act (ACA). The purpose of this article is to clarify misconceptions around how to correctly code a screening completion colonoscopy after a positive first-order test, such as FIT (fecal immunohistochemical test), stool DNA/Cologuard, or blood-based options.
Unfortunately, despite our nation-leading coding guidelines, incorrect coding based on our state’s laws continues to result in inappropriate cost-sharing for patients, therefore increasing the financial burden for patients and creating unnecessary barriers to screening participation.
Payors are aware of and follow our state’s forward-thinking, pragmatic guidelines. Yet coding for CRC screening services, including colonoscopy, begins with physicians and the coders who support their work. Leadership from the Kentucky-based health systems that employ many providers is critical. Adoption and implementation of our nation-leading coding laws will lead to more completed life-saving CRC screenings.
Kentucky is a unique state regarding CRC prevention and control.
We lead the nation in incidence per 100,000, while simultaneously being the most improved state in the nation for CRC screening, having doubled participation since 2002. So clearly, our job is far from done.
Kentucky leads the nation in young CRC incidence under age 50. Rates are startlingly high both among Black Kentuckians and residents of Eastern Kentucky. If we want to successfully control CRC in our state, then we must prioritize screening high-risk individuals at age 40, on-time screening for average risk individuals at age 45 and administering prompt diagnostic evaluation by colonoscopy if symptoms are present.
In Kentucky, laws around colorectal cancer control also includes a state-based and state-funded program for the uninsured and underinsured, The Kentucky Colon Cancer Screening and Prevention Program. This program follows guidelines set by the American Cancer Society, which identifies 45 as the age to start screening for CRC.[1]
Who Is Eligible for Stool-Based Testing?
When providers and patients engage in shared decision-making and average-risk patients can choose their screening modality, overall participation in CRC screening increases. [1] To be eligible for stool-based testing, patients must be asymptomatic and at average risk.
Patients with symptoms, elevated risks (Crohn’s or colitis), or prior personal histories of colon polyps or cancers require a colonoscopy examination. Stool-based testing is not appropriate for CRC or polyp surveillance. Colonoscopy remains the singular test recommended.
When administered to the correct population (asymptomatic, average-risk, 45 and older), approximately one in seven Cologuard tests and one in ten FITs are positive. Negative first order screenings should repeat screening with their preferred modality at the recommended interval. [2] However, those with a positive first-order test must complete the screening process through completion colonoscopy.
We must recognize that screening completion colonoscopy following a positive screening stool test is not a diagnostic exam, rather an integral part of the screening process for average-risk individuals who choose stool–based testing.
Colon Cancer Screening with Colonoscopy Is a One-Part Test.
When a screening colonoscopy is performed, often polyps (adenomas or other lesions) are identified, removed, and/or biopsied. Regardless of the interventions or findings during that screening colonoscopy, the base code should remain a screening colonoscopy.
This coding sequence is widely followed in the non-Medicare population in Kentucky due to our existing coding requirements, resulting from KRS 304.17A-257. CMS finally followed suit by changing the definition and cost-sharing at the Medicare level in December 2020. [3]
Colon Cancer Screening with Stool-Based Testing Is a Two-Part Test.
When a first-order test is performed and is positive, completion of the screening sequence is performed by colonoscopy. The second part of the testing sequence is best described as a completion screening colonoscopy.
The completion screening colonoscopy for a positive stool test is by no means a diagnostic exam, as the patient continues to have no symptoms and started the process as a normal-risk candidate.
The least followed correct coding sequence is what to do after a positive first-order screening test such as a FIT or a multitarget stool DNA test/Cologuard. Guidance around the correct coding as a screening colonoscopy (rather than a diagnostic code) is provided in the Kentucky Department of Insurance opinion from 2015[4]) [2]. Recall, outside of Medicare, laws governing insurance coverage are managed at a state level, not a national level. Therefore, in the non-Medicare population, state laws around correct coding supersedes national guidelines, again (KRS 304.17A-257).
These are not to be confused with diagnostic colonoscopies which are properly coded when people have abdominal symptoms, evidence of bleeding, unexplained weight loss, abnormal imaging, or some clinical complaint that requires a diagnostic intervention to be performed, in this case, colonoscopy.
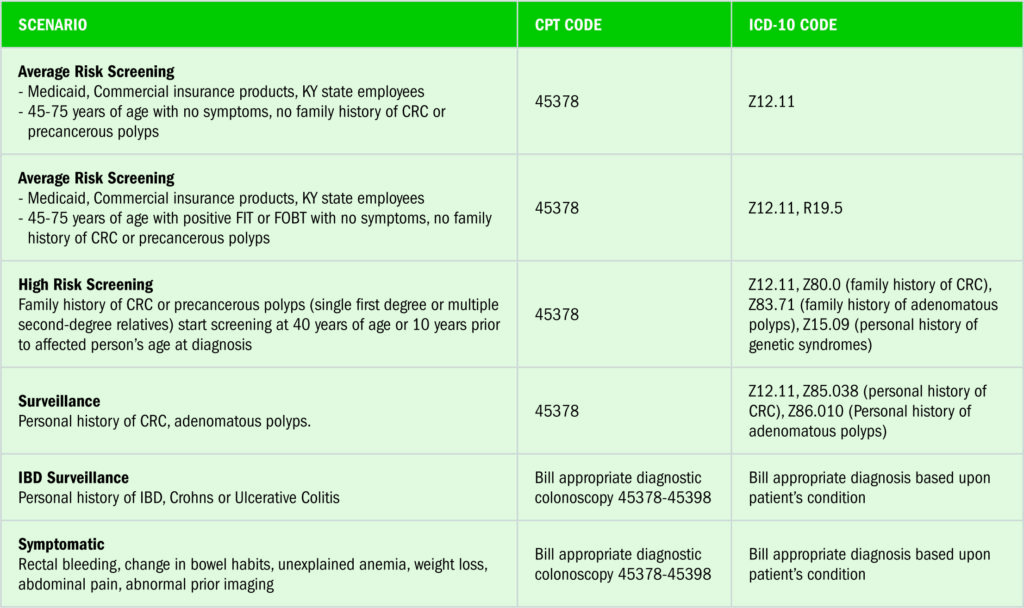
Below are coding tables which may assist you and your team to correct CRC coding for your patients.
Conclusion
Moving forward, we have three major challenges in improving colon cancer screening and inclusion of stool-based testing helps with all of them:
Catch up on the missed screenings during the COVID-19 crisis.
Onboard the 225,000 Kentuckians between 45 and 49 newly eligible for screening via unified guidelines.
Improve screening rates among our neighbors with health disparities or inequities due to socioeconomic, educational, racial, or economic factors.
While we love colonoscopy here in the Bluegrass, to meet our current challenges, we must embrace all options for screening to serve and screen more Kentuckians. Shared decision-making about testing options and correct coding of CRC screening – including the two-part screening process with stool based + colonoscopy for positives – leads to higher screening rates.
Let us work together to get this critical coding component of cancer prevention and control in place for your practice, for your institution (particularly coding partners) and most importantly for your patients.
[1] In mid-2021, USPSTF will be adopting 45 as the recommended starting screening age, therefore, unifying with ACS.
[2] FIT annually, stool-DNA every 3 years, or colonoscopy every 10 years.
[3] https://www.fightcancer.org/releases/house-passes-fix-medicare-cost-sharing-loophole-colorectal-cancer-screenings
[4] https://insurance.ky.gov/ppc/Documents/advop15_03colorectalcancerscreen051215.pdf



